Endoscopic Management of Foreign Body Ingestion: What You Need to Know
- DR Dinesh Vats
- Aug 5, 2025
- 4 min read
Foreign body ingestion is a commonly encountered medical emergency worldwide. It is more prevalent in the pediatric population, accounting for approximately 80% of cases in children aged 4 to 14 years. However, about 20% of cases are seen in adults, often due to accidental ingestion.
Intentional ingestion is most frequently observed in psychiatric patients, such as those with borderline personality disorder. Patients with Pica disorder may ingest non-food items or blunt objects. In elderly individuals, foreign body impaction is often pathological, caused by malignancies, strictures, or motility disorders.
While most foreign bodies pass spontaneously, around 10% to 20% require emergency endoscopic removal.
Classification of foreign body
Category | Sub-category | Examples / Notes |
Radiographic Characteristics | Radiopaque | Appear white or bright on X-ray (block X-rays) |
Radiolucent | Appear dark or invisible on X-ray (allow X-rays to pass through) | |
Blunt Objects |
| Button, coin, toy, battery |
Sharp Objects | Sharp Pointed Objects | Nail, toothpick, needle, safety pin, fishbone |
Sharp Irregular Objects | Partial denture, razor blade | |
Long Objects | Soft Objects | String, cord |
Hard Objects | Toothbrush, ball pen, screwdriver, spoon, fork | |
Food Bolus Impaction | Non Pathological | Bone( Most commonly fish bone) |
Pathological | Malignancy, Stricture, Motility disorders, eosinophilic esophagitis | |
Narcotic Body Packs |
| Intentionally ingested by substance abusers or drug carriers |
Bezoars | Phytobezoar | Plant fibers |
Trichobezoar | Hair (commonly in psychiatric patients) | |
Pharmacobezoar | Undissolved medicines | |
Lactobezoar | Undissolved milk proteins |
Symptoms
In children, history may not always be available. Warning signs include:
Sudden refusal to eat
Drooling
Respiratory symptoms such as coughing or wheezing (suggesting possible aspiration)
In adults, typical symptoms include:
Sudden dysphagia while eating
Odynophagia
Chest pain
Inability to handle secretions
Diagnosis is primarily based on clinical history and physical examination.A plain X-ray is the initial imaging modality of choice to locate radiopaque foreign bodies and to assess for complications such as:
Pneumoperitoneum (air under the diaphragm)
Pneumomediastinum
Pleural effusion
· Management
· Endoscopy is the gold standard for removing foreign bodies.However, in cases with complications like perforation or obstruction, surgical intervention may be necessary.
Do’s and Don’ts in Foreign Body Ingestion
✅ Do’s: Seek immediate medical attention for ingestion of sharp or blunt objects.
Check for airway compromise or respiratory distress.
❌ Don’ts:
Do not give banana, milk, or any food orally – it increases the risk of aspiration and hampers endoscopic visibility.
Do not perform abdominal thrusts (Heimlich maneuver) – especially with sharp objects, as they may cause perforation.
Do not induce vomiting – sharp objects may injure the GI tract during regurgitation.
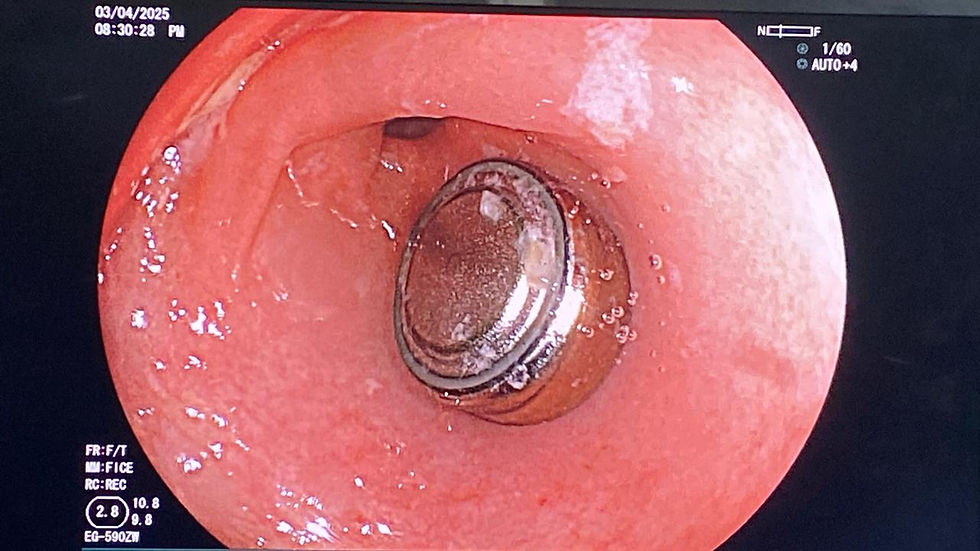
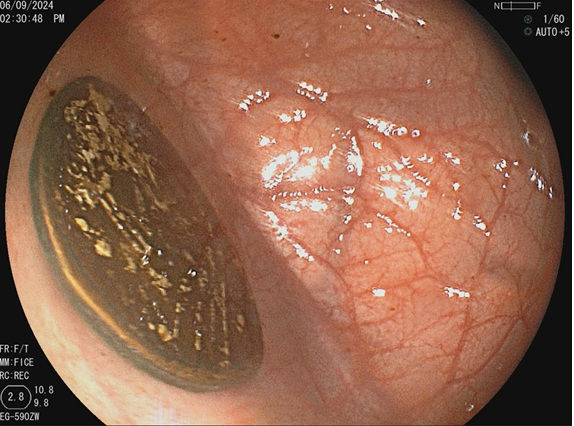
Case Presentations:








Conclusion
Foreign body ingestion is a common yet potentially serious medical emergency that requires prompt recognition and appropriate management. While many cases—especially in children—resolve spontaneously, a significant number necessitate endoscopic intervention to prevent complications such as perforation, obstruction, or infection. Accurate diagnosis through clinical evaluation and imaging, coupled with timely endoscopic removal, is crucial for optimal outcomes. Educating caregivers and the general public on the do’s and don’ts following suspected ingestion can help prevent worsening of the condition. With advancements in endoscopic techniques, most foreign bodies can be safely and effectively removed without the need for surgery.
About the Author
Dr. Naveen Kumar, MBBS, MD, DM (Gastroenterology, PGIMER Chandigarh)Director, Department of GastroenterologySri Harihar Hospital and Research Center, Gutkar, District Mandi, Himachal Pradesh.

Dr. Naveen Kumar is a highly respected gastroenterologist with advanced training from the prestigious PGIMER, Chandigarh. As the Director of the Department of Gastroenterology at Sri Harihar Hospital and Research Center, he brings exceptional expertise in diagnosing and managing a wide spectrum of digestive disorders, with a strong focus on advanced endoscopic techniques.
He is the first and only gastroenterologist in Himachal Pradesh performing endoscopic ultrasound (EUS) and cutting-edge procedures like Peroral Endoscopic Myotomy (POEM) for achalasia cardia, setting new standards in gastrointestinal care across the region.
Renowned for his patient-centered care and commitment to clinical excellence, Dr. Naveen also plays an active role in medical education and public awareness through his writings and academic contributions.
He is the editor of this article, and all endoscopic images included are credited to him.
📧 Email: contact@drnaveenkumargastro.com🐦 Twitter: @drnaveenm



Comments